Blood Thinners and Ginkgo Biloba

Both of these medications are pretty common, but whatever you do, don’t take them together. Blood thinners, especially warfarin, can have a deadly interaction when combined with the herbal product ginkgo biloba. The most dangerous risk is that these two together could cause a person to have an adverse bleeding event.
This is due to the fact that another effect ginkgo biloba has on the body is actually thinning of the blood. That’s like taking two blood thinners! In some cases, doctors who find their patients need a little boost with their blood thinners actually suggest that their patients take both supplements.
HCTZ and Licorice

This isn’t one that most people will think of right off the bat. After all, those who like licorice may not know it actually has medicinal properties that can affect them. The National Health Service suggests that eating as little as two ounces of black licorice for per day can lead to an increase in blood pressure and irregular heart rhythms.
That’s certainly not a great thing for someone that may be taking HCTZ for blood pressure. On top of that, HCTZ is designed to be a diuretic to combat fluid retention, while licorice can cause a person to retain fluid. There may also be additional issues considering licorice can cause potassium depletion.
Antihistamines and Motion-Sickness Medication

Unless you want to feel like someone hit you with a crowbar and you can barely get up, you probably shouldn’t combine antihistamines and Dramamine together. This can cause extreme fatigue and drowsiness that will make it difficult for you to do just about anything – and we certainly wouldn’t recommend getting behind the wheel.
Antihistamines like Benadryl are more likely to produce this undesirable level of fatigue than non-drowsy formulas like Claritin. Both antihistamines and Dramamine are available over the counter but that doesn’t necessarily mean you should do what you want with them. While you may not die, prepare not to get out of bed for the rest of the day if you do take both.
NSAIDs and NSAIDs
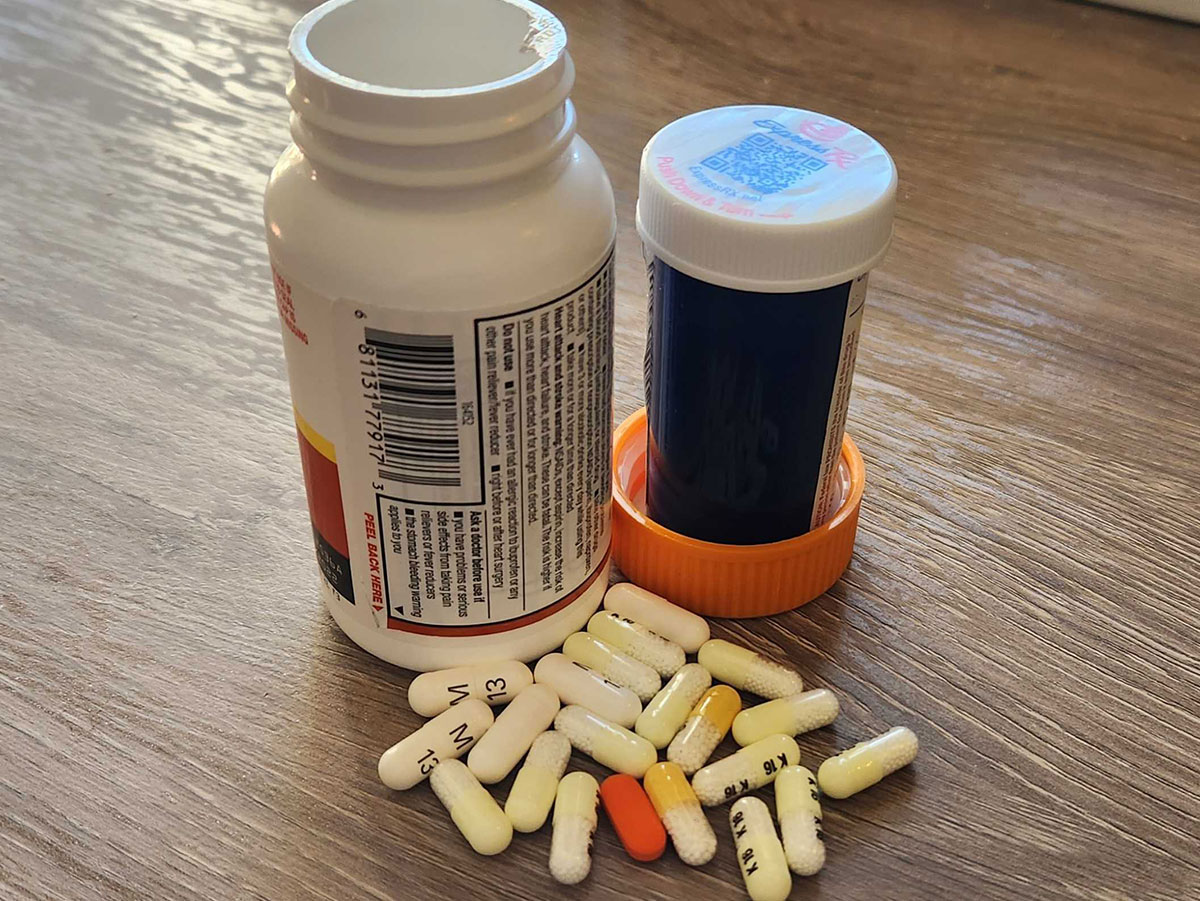
This one may seem like a no-brainer but hear me out. Do you know all products that contain NSAIDs? Spoiler alert: it’s probably more than you think. NSAIDs can go under a variety of names depend on which drug it is including Toradol, Aleve, ibuprofen, Mobic (also known as meloxicam), Motrin, and so many more.
This doesn’t even begin to scratch the surface! It’s really easy to take too many NSAIDs without even knowing it since you can get it over the counter and in prescription form. Taking too much of this medication could cause damage to the stomach lining and stomach bleeding. When in doubt, talk to your pharmacist or doctor to figure out if there is an NSAID in your medications.
Antidiarrheal Medication and Calcium Supplements

This one may be unwittingly easy to overlook, but you should never take antidiarrheal medications and calcium supplements together. The results could be disastrous as you could be faced with some rather severe constipation with the vitamin supplement and medication working together.
The ingredients in antidiarrheal medications slow down intestinal movement while also decreasing the body’s fluid production, reducing your bowel movements. Meanwhile, calcium can firm your stool, making it harder to pass. Thus, when combined, you are left with firm stools that are even more difficult to pass, leading to constipation.
St. John’s Wort and Cold, Flu, & Sinus Relief

St. John’s Wort is an alternative medicine, a shrub native to Europe, whose flowers and leaves contain hyperforin, which can be used to treat depression or menopausal symptoms. But just because it’s a mere alternative medicine, doesn’t mean it doesn’t have some very real side effects when mixed with actual medications.
St. John’s Wort can interact with cold, flu and sinus relief medications like Nyquil by causing a build-up of serotonin in the body. When too much serotonin is built up, you could develop serotonin syndrome, which can manifest in a few different ways, potentially causing diarrhea and body chills, or worse symptoms like fever and even seizures.
Blood Thinners and Ibuprofen

It’s not that blood thinners and NSAIDs like ibuprofen are the same thing, nor even that they accomplish the same thing, but it’s what they can do together that can cause a lot of harm. Ibuprofen is a drug that can cause stomach bleeding, especially when you take too much.
Blood thinners, meanwhile, can increase your risk of bleeding, thus, exponentially increasing your risk of stomach bleeding. When taking blood thinners, your safer bet in terms of NSAIDs is taking acetaminophen, but always talk to your doctor first.
Multi-Symptom Cold and Acetaminophen

Speaking of acetaminophen, never take multi-symptom cold medications with it, as both medications contain acetaminophen. In addition to just not needing extra doses of Tylenol, taking too much acetaminophen can lead to an overdose of acetaminophen, of which the effects can be irreversible.
Taking too much acetaminophen can cause liver damage in the body. This can affect the function of the liver or in cases of severe overdoses can lead to liver damage. It’s understandable to want to feel better when you are sick but trying to kill the pain with acetaminophen is not the way to do it.
Antidepressants and NSAIDs

Antidepressants and NSAIDs can come with an increased risk of bleeding, making these two kinds of medications you may want to avoid taking together. A form of antidepressants called SSRIs with NSAIDs can cause adverse gastrointestinal effects such as stomach bleeding.
SSRIs (selective serotonin reuptake inhibitors) like Zoloft already come with a warning that taking ibuprofen can increase your risk of stomach bleeding. Symptoms can include black stools, rectal bleeding or vomiting blood. And since SSRIs can cause symptoms like headache, it's easy for people to overlook this contraindication.
Vitamin B Complex and Statins
If you want to come out feeling like you just worked out for the first time in months, feeling sore all over, without the benefit of having actually exercised, then by all means, take Vitamin B Complex and Statins together. If not, you may want to avoid taking them together.
When taking any kind of Statins, you should always talk to your doctor before you take any supplements along with it. The combination of Vitamin B3 and statin medication can worsen symptoms of muscle soreness. Together, you and your doctor can determine the cost-benefit of taking both.
Statins and Oral Fungal Medication

Statins and oral fungal medications, like clarithromycin, ketoconazole and itraconazole, can cause increased levels of statins in the blood, which in turn will worsen the side effects of statins. Moreover, it can cause myopathy symptoms such as muscle weakness, cramps, spasms and stiffness.
Additionally, symptoms such as feelings of sickness, insomnia, digestive problems and headache may also be worsened by taking the two types of medications together, especially since antifungal medications can already produce undesirable digestive issues.
HCTZ and Decongestants
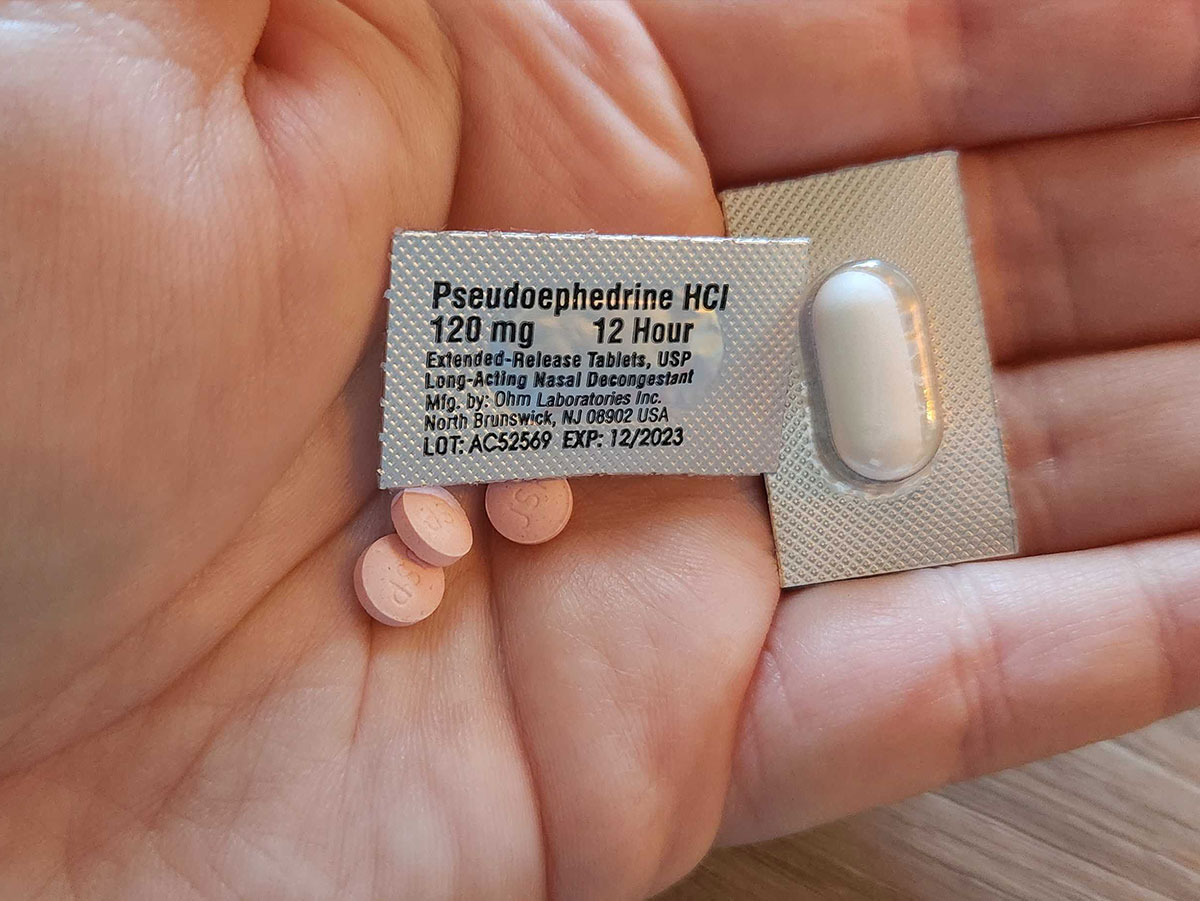
HCTZ is commonly used to treat hypertension, also known as high blood pressure. While using HCTZ and and decongestants are not commonly believed to cause harmful drug interaction, the two drugs don’t really mix nonetheless. When combined, the two medications can pose a risk for people with hypertension.
Decongestants such as pseudoephedrine, phenylephrine, ephedrine and naphazoline can increase your blood pressure and heart rate which means your blood pressure medication won’t work as well. On thart same note, you want to avoid medications that are high in sodium as sodium also raises blood pressure.
Statins and Grapefruit Juice

Statins are medications that are designed to lower your cholesterol. Drinking grapefruit juice can affect statins by increasing the level of statins in your blood. As a result, you could be faced with worsened side effects while taking statins. While the delicious juice is high in vitamin C and potassium, it just doesn’t quite mix with your meds.
In addition to statins, grapefruit juice should not be taken with several other medication types, such as high blood pressure medications, anti-anxiety drugs, and corticosteroids just o name a few. It's also important to note that the severity of interactions can vary from person to person, so talk to a doctor first.
St John’s Wort and Antidepressants

Because of St. John’s Wort’s potential therapeutic benefit in treating depression in some patients, taking it with some actual antidepressant drugs can have a detrimental effect, once again causing increased serotonin levels in the body, potentially causing serotonin syndrome.
Serotonin syndrome can produce a number of symptoms including mild ones like agitation, insomnia, confusion to more severe symptoms like rapid heart rate, loss of muscle coordination and high blood pressure. Severe serotonin syndrome symptoms include seizures, irregular heartbeat and unconsciousness. Talk to your doctor before using St John’s Wort and antidepressants at the same time.
Antidepressants and Antihistamines

Antidepressants, like SSRIs and SNRIs, and antihistamines can interact thanks to their effects on neurotransmitters in the brain. They can increase your risk of serotonin syndrome, which occurs when there are high levels of serotonin in the brain. This can cause a ton of potential problems, such as high fever, rapid heart rate and confusion.
Additionally, both medications may cause increased levels of drowsiness, making it unsafe for you work work around or operate machinery, or especially drive a car. It is best to avoid taking these medications at the same time, but you may take them spread apart. However, talk to your doctor first.
Anti-Seizure Drugs and Alcohol

The anti-seizure and anti-anxiety medication known as lorazepam is not safe to mix with alcohol – before, after, nor during. Alcohol can intensify the side effects of lorazepam, which can potentially lead to life-threatening events or circumstances. You should NEVER mix these two drugs.
Alcohol can intensify lorazepam’s most serious side effects. In some cases, it can cause slowed breathing which can have potentially fatal consequences. Mixing lorazepam and alcohol can reduce your cognitive abilities and it is advised that you wait at least 100 hours after taking lorazepam to consume alcohol.
NSAIDs and Alcohol

NSAIDs and alcohol are usually a bad combo. As mentioned earlier, NSAIDs usually come with the risk of stomach bleeding, especially when you take too many. Drinking while taking NSAIDs can increase stomach irritation, while also increasing your risk of stomach bleeding.
Taking acetaminophen and drinking too much alcohol can have detrimental effects on your liver. Both drugs come with the risk of liver damage, so taking both at the same time ups the ante, exponentially. You should always wait for the acetaminophen to leave your body before you start drinking again.
ADHD Drugs and Alcohol

ADHD drugs like amphetamine and dextroamphetamine, also known as Adderall, can be used to treat attention deficit hyperactivity disorder or narcolepsy. It can affect the chemicals and nerves in the brain that contribute to impulse control. You should never drink alcohol with Adderall together as the effects can be dangerous.
The effects of taking both have unpredictable effects. Its not a matter of cancelling each other out, either. One drug can cancel out the other or change the other drug’s desired effect. Ultimately, symptoms can mask just how much you’ve taken and thus you are more likely to take more and overdose. On top of this, it can increase your risk of cardiovascular problems, respiratory infection and heart failure.
Anticoagulants and Grapefruit Juice

It’s not just statins. You should never drink grapefruit juice while taking anticoagulants like warfarin. The grapefruit juice can amplify the effects of warfarin on your blood, causing you to bleed more profusely, particularly in the case of an injury but not limited to that.
One possible side effect of warfarin is internal bleeding. While rare, internal bleeding risk may be increased by drinking grapefruit juice at the same time as warfarin. Signs of internal bleeding can include severe headache, bloody urine or stool, and even nosebleeds.
Blood thinners and Vitamin K-Rich Foods

Blood thinners like warfarin should not be consumed with foods that are rich in vitamin K. Leafy greens like kale and even broccoli pack a ton of vitamin K and should especially be avoided. The main concern is that vitamin K can negate the effects of warfarin, causing it not to work.
So, the good news is that if you hate eating your broccoli, you might be in luck because this is the one time your doctor won’t recommend it. Vitamin K can increase your risk of blood clotting, thus increasing your risk of heart attack and stroke, for which the warfarin is usually prescribed to prevent.
Hypothyroid Drugs and Any Food

Hypothyroidism occurs when the thyroid gland can’t sufficiently produce enough hormones to meet your needs, which can slow your metabolism and make you feel tired. Often medication is prescribed for this condition but it's important to take it as directed.
Medication can restore your hormone levels when taken regularly but there’s a reason you are instructed to take it up to an hour before eating. It turns out that food can block the absorption of the drug in your small intestine, so it won’t work properly. And yes, coffee and milk count as food too.
Blood Thinners and Antacids

Antacids, including over-the-counter options, can interact with some blood thinners, more specifically, warfarin. Bismuth subsalicylate, also known as Pepto-Bismol or omeprazole, can cause increased bleeding as a result of taking warfarin, as antacids can enhance its effects.
Major bleeding events can occur from even minor injuries since blood clotting is essential for the body in stopping bleeding. While blood clotting medications are designed to prevent larger clots from forming in the body, they aren’t designed to stop clotting altogether.
Nicotine and Insulin

Nicotine and insulin are two other drugs that just don’t get along. Smoking or even putting on a nicotine patch can have a dangerous effect on diabetic individuals. Insulin is often prescribed for diabetic patients who need more insulin in the body to control blood sugar levels, but nicotine counteracts that.
While nicotine won’t exactly reduce the insulin in your bloodstream, it will change your blood cells and their ability to respond to insulin. Therefore, the insulin will not be able to turn your food into energy and you will be faced with increased blood sugar, which can damage your body’s organs and blood vessels.
Blood thinners and Sulfa Drugs

Sulfa drugs are some of the most common antibiotics available for a variety of uses. Using warfarin and sulfa drugs can increase your risk of bleeding, especially in elderly individuals with kidney or liver problems. Interaction between these drugs is possible as sulfa drugs can affect the body’s ability to process the blood thinner properly.
Bleeding may occur from your gums or nose in many cases. It might also manifest as bruising or dark stools, indicating that you are suffering from internal bleeding. While these are risks, ultimately it may be between you and your doctor to discuss whether the benefits outweigh the costs.
Turmeric and Blood Thinners

Turmeric can be a miracle spice in many individuals due to its numerous health benefits. It can reduce inflammation and prevent numerous diseases, including heart disease, liver disease and respiratory infections – just to name a few. But if you are taking blood thinners, you may want to avoid turmeric.
Turmeric can be used in cooking or even taken as a supplement. But you want to avoid supplemental quantities if you are taking blood thinners as turmeric can already reduce clotting in the body. It’s anti-clotting properties will work in combination with your blood thinner, increasing your risk of bleeding.
CoQ10 and Blood Thinners

CoQ10 is an antioxidant in the body that promotes cell maintenance and growth. As we get older, our levels of it decrease which is where supplements come into play. However, if you are taking blood thinners, you’ll want to avoid taking CoQ10 supplements, whether taken as a capsule, tablet or syrup.
Although it can be great for those suffering from diabetes, migraines or heart disease, CoQ10 can affect a blood thinner’s ability to work properly. It can actually prevent the blood thinner from working, allowing blood clots to form and potentially cause heart attack and stroke.
Chemotherapy and Vitamin C

Those undergoing chemotherapy should not take vitamin C supplements or consume foods rich in vitamin C as the nutrient can affect chemotherapy’s effectiveness. Vitamin C is rich in fruits like oranges, berries, tomatoes and broccoli. And while it can prevent cancer when you don’t have it, it can cause problems if you are trying to treat it.
High doses of vitamin C will not only prevent chemotherapy from working as well, but it can also affect estrogen hormone levels and statins. Some studies have shown improved quality of life for patients on chemo, but more research is needed. Always talk to your doctor before making any major dietary changes.
Milk Thistle and Insulin

Milk thistle and insulin is another bad combo. Milk thistle, a flowering plant closely related to daisies can be ingested to promote heart and liver health. As a supplement, it can also reduce blood sugar. However, you shouldn’t use it at the same time you are taking insulin.
Diabetic patients may be thinking they are doing themselves a favor but by taking milk thistle supplements, you can end up overdoing it in terms of blood sugar levels, ending up with low blood sugar. Low blood sugar can cause problems such as rapid heartbeat, anxiety dizziness, hunger and confusion.
St. John’s Wort and Migraine Medication

St. John’s wort is at it again, this time interacting with migraine medicine, but more specifically, triptans like sumatriptan. When combined, the supplement can increase serotonin levels in the body, which can cause a variety of side effects from mild to severe.
Serotonin toxicity can be potentially life-threatening. Signs can include diarrhea, shaking, fever or muscle rigidity. It can also cause seizures. And that risk aside, ultimately St. John’s wort can worsen migraines in some patients. That’s why you should always talk to your doctor before taking a new supplement.
Dairy and Antibiotics

You should never consume dairy while taking certain antibiotics. Diary includes all the good stuff like cheese, yogurt, ice cream, butter and milk. These dairy products can bind themselves to your antibiotic medication and affect its ability to absorb in the bloodstream.
You should avoid consuming dairy two hours before and six hours after taking your antibiotics as they will not work. On that same note, if you are taking yogurt for your gut, you want to wait at least two hours so that the antibiotics do not kill the good bacteria you are trying to take in.
 Author
Sherrill Dean
Last Updated: January 16, 2026
Author
Sherrill Dean
Last Updated: January 16, 2026